Portable and affordable
Respond to pandemics
Used for wide range of conditions
Identify “silent hypoxia”
Many clinical conditions can result in hypoxemia, including acute respiratory illnesses like pneumonia and COVID-19, newborn conditions, complications during childbirth, asthma, and heart failure. Every year, nearly 5 million children die before their first birthday, with respiratory distress being one of the leading causes. Hypoxemia is a potentially fatal complication of severe pneumonia, the leading infectious cause of death for children under 5.
The World Health Organization (WHO) recommends pulse oximeters for primary health care as part of integrated management of childhood illness. However, primary health care workers in many low-resource settings rely on clinical signs, such as rapid breathing or shortness of breath, for triaging and treatment. There are known issues with the accuracy and reliability of relying on clinical signs; these issues result in many patients being misdiagnosed and not receiving appropriate care. Patients may receive medicines that they don’t need, including antibiotics, which in turn, can lead to antimicrobial resistance.
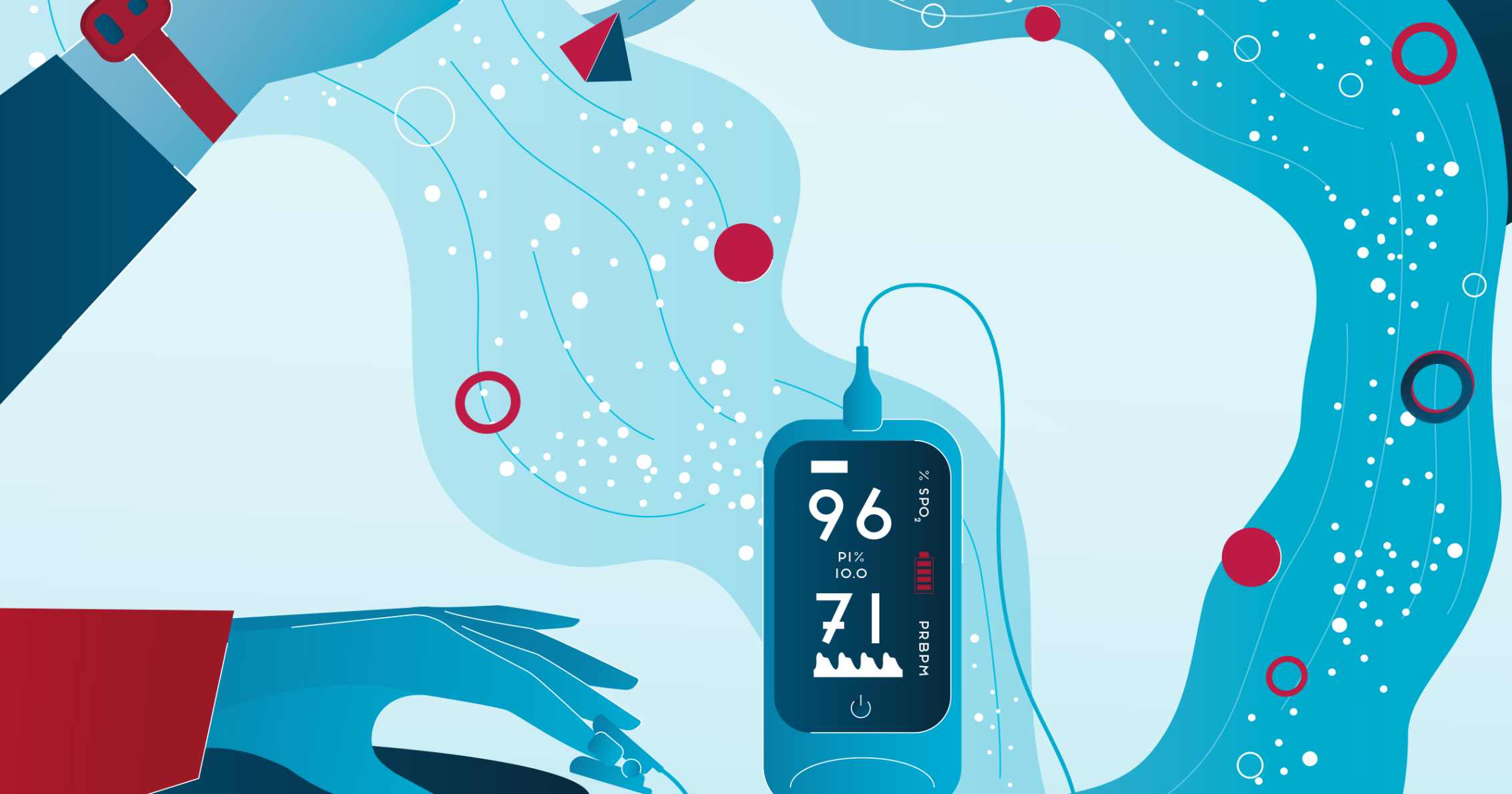
Pulse oximeters are noninvasive devices that measure blood oxygen saturation and pulse rate. They are used to help health care workers detect hypoxemia – a low level of oxygen in the blood – and to know how much medical oxygen to administer to patients. While pulse oximeters that fit on a patient’s finger are the most common, there are several other types including hand-held, phone-based, and wearable models. When fingertip sensors don’t work well for infants or very young children, there are alternatives like toe sensors, earlobe sensors, or even wrap-around foot sensors that ensure more accurate readings despite smaller body parts or more delicate skin.
Because they are portable and non-invasive, pulse oximeters are particularly suitable for use at the primary care level. Detecting hypoxemia can allow timely treatment, including with oxygen therapy when needed, and save hundreds of thousands of lives each year. For example, during the COVID-19 pandemic, pulse oximeters were crucial for triaging COVID-19 patients and identifying those in need of urgent care and medical oxygen therapy, especially when hospital resources were scarce.
Pulse oximeters are an essential component of a strong health system. Understanding technological challenges, existing and pipeline products, and market challenges is key for facilitating equitable access to pulse oximeters and for Unitaid’s efforts to support countries to address medical oxygen gaps in their health systems in line with the WHO resolution on increasing access to medical oxygen in 2023. To help enable the scale-up of pulse oximeters in primary health care, Unitaid supported research to evaluate the feasibility, cost-effectiveness and impact of expanding the use of pulse oximeters for use by primary health workers in low-resource settings. The studies demonstrated good acceptance of pulse oximeters by health care providers and showed that to improve health outcomes, introduction of pulse oximeters needs to be integrated as part of “whole of systems” approach and not as a standalone intervention.
Unitaid and PATH also published the “Next generation pulse oximeters: technology and market landscape report” in 2022, which assessed the potential of multimodal pulse oximeter devices – devices that can measure oxygen levels and other vital statistics like respiratory rate, temperature, and/or hemoglobin – to improve the integrated diagnosis and treatment of illnesses for patients presenting at health facilities in low- and middle-income countries, with a focus on maternal and child health. During the COVID-19 pandemic, we delivered more than 5,000 pulse oximeters to health facilities in low- and middle-income countries. Through our support for the Open Oximetry Project, we have also worked to address challenges in existing pulse oximeters that have been shown to overestimate oxygen saturation in the blood of patients with darker skin pigmentation – which can lead to delayed or inadequate medical treatment, with potentially fatal consequences.